Last Updated on November 27, 2025 by Noria ALHUSAM
Introduction:
Coronary artery disease (CAD), is one of the most common and serious heart conditions. It arises from a dysfunction in the coronary arteries, which supply the heart with oxygen-rich blood.
Definition of Coronary Arteries
Coronary arteries, are the primary blood vessels that deliver oxygen-rich blood and nutrients to the heart muscle, ensuring that it performs its vital functions efficiently including pumping blood throughout the entire body. These arteries originate from the aorta and branch into the right coronary artery and left coronary artery, which in turn divide into smaller arteries that penetrate the heart muscle to meet its continuous needs.
How Does Coronary Artery Disease Develop?
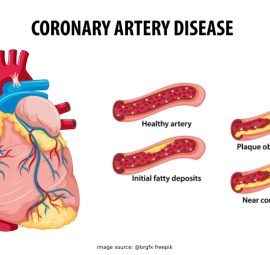
Coronary artery disease, develops gradually over the course of years and is one of the most prevalent forms of heart disease. Most heart attacks are attributed to this condition. It occurs when blood flow to the heart muscle is reduced due to the buildup of fats, cholesterol, and other substances (such as cellular waste and fibrin) on the arterial walls—a condition known as atherosclerosis.
This buildup is called plaque, and over time it leads to the narrowing of the arteries and the obstruction of blood flow. In some cases, a person may not experience any symptoms until a heart attack occurs especially if a plaque ruptures, forming a blood clot that can fully block the artery. While this process can take years, it may ultimately result in a heart attack or heart failure.
Is Coronary Artery Disease a Modern Disease?
Although often associated with modern lifestyles, historical studies have shown that atherosclerosis has existed for thousands of years. CT scans of mummies from ancient Egypt, Peru, and the Pueblo and Unangan peoples revealed signs of atherosclerosis in 34% of 137 mummies—dating back over 4,000 years.
Today, the prevalence of coronary artery disease varies globally. In high-income countries such as the United States, Western Europe, and Australia, the highest rates of incidence are recorded. In the U.S. alone, 18.2 million people are affected, and there were 375,476 deaths linked to the disease in 2021.
In regions like South Asia, the Middle East, and North Africa, the disease is widespread due to genetic factors, poor nutrition, and high rates of obesity and diabetes. Similarly, Eastern Europe and Russia report high rates due to smoking and unhealthy dietary habits. Meanwhile, urban areas in sub-Saharan Africa are beginning to see a gradual rise in incidence.
Despite medical advancements, the disease remains a global health challenge. Sedentary lifestyles, diet globalization, and decreased physical activity have contributed to rising rates of CAD—especially in developing countries undergoing social and behavioral transformations.
Why Is Coronary Artery Disease So Important?
- Coronary artery disease (CAD), is among the most widespread cardiovascular conditions and a leading cause of death globally, affecting millions of people each year. It can result in serious complications such as heart attacks, angina, and heart failure.
In the United States alone, more than 20 million individuals live with CAD, and the disease accounts for one in every four deaths. - CAD imposes a significant economic burden due to the high costs of treatment and care, in addition to reduced productivity caused by premature death or chronic disability.
This underscores the importance of prevention and early intervention to reduce both incidence and mortality rates and to lessen the broader economic consequences.
Causes and Contributing Factors to Coronary Artery Disease (CAD):
Coronary artery disease occurs due to the accumulation of plaques inside the arteries supplying blood to the heart. These plaques are composed of cholesterol, fats, calcium, and inflammatory cells, which narrow the arteries and restrict blood flow.
Main Causes: What Chokes Your Arteries?
Although cholesterol is the common culprit, the truth is more complex. Here are the primary causes of atherosclerosis:
-
Disorders of Cholesterol and Lipid Metabolism
These disorders affect how the body handles fats and cholesterol and result from deficiencies or malfunctions in enzymes or receptors responsible for cholesterol regulation. They may be genetic or acquired:
-
a) Genetic (Inherited) Disorders:
- Familial Hypercholesterolemia (FH): Caused by defects in LDL receptors, preventing efficient clearance of LDL cholesterol.
- Genetic mutations in PCSK9 or Apolipoprotein B: Lead to abnormally high levels of harmful cholesterol.
- Beta-lipoproteinemia and hepatic lipase deficiency: Rare conditions impairing lipid breakdown and transport in the blood.
- Sitosterolemia: Impairs elimination of plant sterols, causing their accumulation alongside cholesterol.
-
b) Acquired (Non-genetic) Disorders:
- Liver diseases such as cholestasis: Prevent bile secretion and cause severe cholesterol elevation (>1000 mg/dL).
- Endocrine disorders like hypothyroidism: Reduce lipid metabolism.
- Certain medications: Such as steroids and diuretics, may raise cholesterol levels.
- Other cardiovascular diseases: Such as arterial pathologies.
-
Chronic Inflammation and Atherosclerosis
Chronic inflammation plays a major role in heart and artery diseases. When the arterial lining is damaged by inflammation, it triggers an immune response leading to the accumulation of foam cells (lipid-laden macrophages), which gradually form fatty plaques inside the artery walls.
As inflammation worsens, plaques thicken and enlarge, narrowing the arteries and impeding normal blood flow. The danger does not stop here — inflammation also makes these plaques more fragile and prone to rupture. When plaques rupture, blood clots may form and fully block the artery, potentially causing sudden heart attacks.
Key triggers of this chronic inflammation include:
- Insulin resistance: Elevates blood sugar and insulin levels, stimulating inflammatory cytokines (e.g., IL-6, TNF-alpha), damaging the vascular endothelium. It is also linked with high triglycerides and low HDL cholesterol, increasing atherosclerosis risk.

- Excess body weight, especially abdominal fat: Usually associated with insulin resistance; fat tissue secretes inflammatory cytokines accelerating artery stiffening.
- Reduced nitric oxide (NO): A compound that normally dilates blood vessels, its levels drop with inflammation and insulin resistance, raising the risk of stiffness and hypertension.
- Immune and microbiome disturbances: Cause ongoing immune activation. Dysbiosis may allow harmful gut particles into the bloodstream, perpetuating chronic immune alertness and fueling inflammation that leads to heart disease.
-
Imbalanced Immune Response
Immune cells play a pivotal role in atherosclerosis by reacting excessively to vascular injury.
When arteries are damaged, immune cells engulf harmful cholesterol and become foam cells, leading to fibrous tissue and calcium deposition, forming scars or plaques on arterial walls to repair damage. However, when this immune response is excessive or imbalanced, it causes the formation of atherosclerotic plaques — foam cells grow large and rigid inside artery walls, narrowing the arteries and impairing blood flow.
This process can result in heart attacks or stroke if plaques rupture. Immune dysfunction also decreases nitric oxide and disturbs lipid balance, further increasing disease risk.
Core Risk Factors
-
Lifestyle-Related Risk Factors (Modifiable)
- Unhealthy diet: High intake of saturated fats and sugars, low in vegetables and fiber, leads to elevated cholesterol.
- Physical inactivity and obesity: Increase insulin resistance and abdominal fat accumulation, raising the likelihood of hypertension and harmful cholesterol, thereby elevating heart disease risk.
- Chronic kidney disease: Long-term kidney ailments increase coronary artery disease risk.
- Chronic stress and psychological pressure: Raise blood pressure and stress hormones like cortisol, negatively impacting heart health.
- Sleep quantity: Both insufficient and excessive sleep are linked to higher heart disease risk.
- Excessive smoking: Reduces oxygen delivery to the heart and promotes inflammation, increasing atherosclerosis risk.
- Excessive alcohol intake: Raises blood pressure and triglycerides, elevating heart disease risk.
- Poor control of chronic diseases: Such as hypertension, diabetes, high cholesterol, and chronic kidney disease, exacerbates coronary artery disease risk.
-
Non-Modifiable Risk Factors (High-Risk Groups)
- Age: Coronary artery disease prevalence increases with age due to vascular stiffness and plaque buildup, beginning to rise notably after age 35 in both men and women. Studies indicate risk after age 40 is approximately 49% for men and 32% for women.
- Sex: Men are more prone before women reach menopause. Female hormones provide some protection until menopause.
- Ethnicity: Black, Hispanic, Latino, and Southeast Asian populations face higher coronary artery disease and mortality risk compared to other ethnic groups.
- Family history: A major risk factor. Individuals with first-degree relatives diagnosed with early heart disease (father or brother before 55 years, mother or sister before 65 years) have increased risk and mortality.
Other Mechanical or Physiological Factors
-
Non-atherosclerotic heart or vascular diseases:
- Aortic valve stenosis or regurgitation: Stenosis forces the heart to pump against increased resistance, raising workload and oxygen demand. Regurgitation causes volume overload, similarly increasing cardiac workload and oxygen needs. Both lead to cardiac hypertrophy and reduced diastolic time, impairing oxygen supply despite patent coronary arteries.
- Severe anemia: Reduces blood oxygen-carrying capacity. To compensate, the heart increases output by raising heart rate and contraction strength, increasing myocardial oxygen consumption while oxygen supply per beat decreases. This can cause relative myocardial ischemia and angina symptoms, especially with pre-existing coronary narrowing. Although anemia does not cause atherosclerosis, it is an indirect risk factor by increasing cardiac metabolic burden.
- Tachycardia: Sudden episodes of fast heart rate shorten diastole (coronary blood flow phase), reducing oxygen delivery to the heart and increasing oxygen demand. Severe tachycardia lowers coronary reserve and can trigger ischemia (angina) even without coronary artery stenosis, acting as an indirect trigger for acute coronary syndrome.
- Hyperthyroidism: Elevated thyroid hormones increase basal metabolic rate and heart activity, causing faster and stronger heartbeats with higher oxygen demand. This mismatch can cause myocardial stress and ischemia even if coronary arteries are clear. Thus, hyperthyroidism is an indirect risk factor raising cardiac metabolic demand.
These mechanical and physiological conditions increase myocardial oxygen demand or reduce supply relatively without directly causing atherosclerosis but exacerbate coronary artery disease symptoms.
Additional Risk Factors for Coronary Artery Disease
- Obstructive sleep apnea: Causes intermittent oxygen deprivation during sleep, increasing cardiac workload and blood pressure, raising heart disease risk.
- High sensitivity C-reactive protein (hs-CRP): Marker of chronic inflammation directly linked to atherosclerosis.
- Elevated triglycerides: Especially in women, a significant risk factor for coronary artery disease progression.
- Increased homocysteine: An amino acid whose high levels cause vascular damage and promote atherosclerosis.
- Preeclampsia: A pregnancy complication causing hypertension and vascular injury, increasing future heart disease risk.
- Other pregnancy complications: Gestational diabetes or hypertension indicate higher future cardiovascular risk.
- Autoimmune diseases: Such as lupus and rheumatoid arthritis, accompanied by chronic inflammation increasing atherosclerosis risk.
- HIV/AIDS: Patients face higher atherosclerosis and coronary artery disease risk due to chronic inflammation, antiretroviral therapy effects, and accelerated vascular aging.
- Body Mass Index (BMI) over 25: Indicates overweight or obesity, increasing hypertension, type 2 diabetes, and dyslipidemia risk, all direct coronary artery disease risk factors. Obesity also promotes chronic inflammation and insulin resistance.
- Early menopause (before 40 years): Loss of estrogen’s protective effect early increases coronary artery disease risk compared to menopause after age 50.
- Endometriosis: This chronic inflammatory disease is linked to higher coronary artery disease risk, possibly due to systemic inflammation, hormonal influences, and vascular effects of the disease and treatments.
Forms of Coronary Artery Disease
Coronary artery disease is not limited to one type. It includes several clinical forms that differ in their mechanism, severity, and impact on blood flow to the heart muscle.
Some of the most prominent forms of coronary artery disease are:
-
Stable Ischemic Heart Disease
In this pattern, the heart has difficulty getting enough oxygenated blood during physical exertion or emotional stress.
This is due to progressive narrowing of the coronary arteries.
It manifests as stable angina pectoris — a pain or pressure in the chest that usually subsides with rest or the use of artery-widening medications such as nitroglycerin.
-
Acute Coronary Syndrome (ACS)
ACS is a cardiac emergency caused by a sudden and severe decrease in blood flow to the heart muscle.
It is often triggered by the rupture of a fatty plaque within the coronary artery.
This rupture leads to the formation of a blood clot that blocks the bloodstream.
Acute coronary syndrome includes three main conditions that vary in severity:
- Unstable angina.
- Non ST-segment elevation myocardial infarction (NSTEMI).
- ST-segment elevation myocardial infarction (STEMI).
These conditions require urgent medical intervention.
Delayed treatment can lead to permanent damage to the heart muscle or even death.
-
Atherosclerotic Coronary Artery Disease
This form is caused by the gradual buildup of fatty plaques within the walls of the coronary arteries.
These plaques are composed of cholesterol, inflammatory cells, and fatty substances.
They cause narrowing and hardening of the arteries.
This narrowing limits the flow of oxygen-rich blood to the heart muscle, especially during exertion.
Over time, it can lead to heart attacks or strokes.
You’re more likely to develop this type of disease if you have risk factors such as:
- High LDL cholesterol (bad cholesterol).
- Smoking.
- Type 2 diabetes.
- Chronic insulin resistance.
- High blood pressure.
- Obesity or physical inactivity.
Symptoms of Coronary Artery Disease
The symptoms of coronary artery disease vary depending on the stage and severity of the arterial blockage.
They can be categorized into two main types:
Acute Symptoms
These are sudden and serious symptoms that require urgent medical intervention.If not treated immediately, they can lead to a heart attack, heart failure, or even death.
These symptoms include:
– Severe chest pain or pressure (unstable angina), which:
-
- May radiate to the left arm, neck, jaw, or back.
- Lasts more than 10–15 minutes.
- Does not improve with rest or typical medications.
- Is often accompanied by shortness of breath, extreme fatigue, and excessive sweating.
- May also be accompanied by nausea, dizziness, or fainting.
Unstable angina is a medical emergency.
It requires immediate hospitalization, as it may be a precursor to a heart attack.
– Heart Attack – Myocardial Infarction:
Occurs when one of the coronary arteries is completely blocked.
Symptoms include:
- Severe or pressing chest pain.
- Pain spreading to the shoulder, arm, back, neck, or jaw.
- Nausea, profuse sweating, shortness of breath, and sudden dizziness.
Note: In women, the elderly, and diabetics, symptoms may be atypical, such as: extreme fatigue, heartburn, pain in the back or jaw only, or even without obvious pain.
– Sudden swelling of the legs or abdomen with difficulty breathing
May indicate acute pulmonary edema due to acute heart failure.
– Severe palpitations or heart rhythm disturbances (Arrhythmias):
May be indicative of serious electrical dysfunction of the heart due to ischemia.
Chronic or Secondary Symptoms:
Occur gradually and are not immediately life-threatening, but indicate an issue that needs medical follow-up and treatment to prevent complications.
They include:
- Stable Angina: Pain or tightness in the chest that occurs during physical exertion or emotional stress and improves with rest or artery-dilating medications.
- Dyspnea: Especially when walking or climbing stairs, may indicate progressive heart failure.
- Unexplained fatigue or general weakness: Due to inadequate perfusion of oxygen-rich blood to the muscles and tissues.
- Mild swelling of the feet or ankles: A result of fluid retention, and may be an early sign of heart failure.
- Mild palpitations or a temporary irregular heart rhythm: Due to the lack of blood supply to the heart.
- Mild dizziness or occasional loss of balance.
Coronary Artery Disease Symptoms in Women:
Women tend to experience less pronounced or different symptoms than men, especially during a heart attack.
These include:
- Mild or nonspecific chest pain.
- Shortness of breath.
- Unusual and severe fatigue.
- Nausea or vomiting.
- Back, jaw, or shoulder pain.
- A general feeling of illness without obvious chest pain.
Ignoring these symptoms can lead to delayed diagnosis and increased complications.
Impact of Coronary Artery Disease on General Health
This disease leads to impaired heart and circulatory functions, resulting in a range of serious health effects, including:
- Reduced Heart Performance: Narrowing of the coronary arteries leads to decreased blood flow to the heart muscle, causing angina or a heart attack.
- Problems in the Circulatory System: Blood pressure increases due to the extra effort required by the heart to pump blood through the narrowed arteries. This may lead to fluid accumulation in the limbs and lungs, resulting in congestive heart failure.
- Reduced Level of Physical Activity: Patients experience fatigue and shortness of breath during daily activities due to inefficient blood pumping, which decreases their ability to engage in regular tasks.
- Increased Risk of Serious Complications: Such as heart failure caused by poor blood flow to vital organs, and arrhythmias like atrial fibrillation, which may cause fainting or a stroke if a blood clot travels to the brain.
- Impact on Quality of Life: Patients suffer from limitations in physical and social activities due to symptoms like pain, fatigue, and shortness of breath, which reduces their daily well-being.
- Psychological Impact: Anxiety and depression are common among coronary artery disease patients due to health limitations and fear of complications.
Treating and Preventing Coronary Artery Disease Naturally
Smart nutrition, lifestyle, and integrated arterial support.
First: Prevention of Coronary Artery Disease (healthy people)
1. Preventive Nutrition:
- Minimize sugars and harmful fats; avoid processed foods and fast food.
- Load up on antioxidant-rich fruits and vegetables (e.g., berries, broccoli, red peppers).
- Use healthy fats, such as olive oil, avocado, and flaxseed.
- Eat garlic and onions, as they contain compounds and antioxidants that help clean the arteries and improve blood flow.
- Add turmeric, for its role in raising good cholesterol (HDL) and lowering bad cholesterol (LDL).
- Drink ginger decoction or add it to food, as it has anti-inflammatory and artery-dilating properties.
- Focus on foods that promote the production of nitric oxide (such as beets and pomegranates), to improve vasodilation.
2. Physical Activity:
- Regular moderate aerobic exercise such as brisk walking, swimming, or cycling.
- Exercise improves blood flow, reduces inflammation, and stimulates stem cells to repair the lining of the arteries.

3. Daily Health Habits:
- Early and deep sleep, which is associated with regenerating heart tissue and stimulating stem cells.
- Avoiding smoking and minimizing stress are important factors in protecting against narrowing of the arteries.
- Intermittent fasting for 12 to 16 hours reduces inflammation and stimulates tissue repair.
4. Regular Check-Ups
5. Perform Tests to Assess Arterial Health:
- Measuring small LDL particles
- Analyzing insulin resistance
- Regularly monitor blood pressure, cholesterol, and blood sugar
- Early detection of chronic inflammation or signs of calcification
secondly: Coronary Artery Disease Treatment (for Patients)
Foods That Clean the Arteries and Support the Heart
1. Therapeutic Food
- Garlic, onions, turmeric, fresh ginger, and beets:
Garlic and onions are two of the most powerful heart-healthy foods. They contain sulfur compounds that activate liver detoxification enzymes and reduce oxidative stress and inflammation associated with atherosclerosis. They also help improve blood fluidity, reduce excess clotting in a natural and safe way, as well as improve insulin sensitivity and blood lipid balance.- Garlic helps eliminate cholesterol by stimulating the secretion of bile.
- Onions promote the production of nitric oxide, which helps lower blood pressure and dilate blood vessels.
- Turmeric, ginger, and beets:
These foods have unique properties in supporting circulation and strengthening the heart muscle.- Turmeric contains curcumin, an anti-inflammatory compound that supports blood vessel elasticity and reduces oxidation.
- Ginger improves blood flow, reduces platelet buildup, and reduces inflammation.
- Beets are rich in natural nitrates that convert into nitric oxide, dilating blood vessels and lowering blood pressure — crucial for reducing the burden on the heart and coronary arteries.
- Traditional remedy:
A mix of small tomatoes + olive oil + yogurt + crushed garlic — known for its ability to dilate vessels and dissolve small clots. - Green tea, purslane, sunflower seeds:
These foods show clear benefits in supporting arterial and heart health.- Green tea contains catechins, powerful antioxidants that reduce inflammation, improve endothelial function, and reduce oxidation of LDL cholesterol, thereby slowing atherosclerosis progression.
- Legumes are rich in omega-3 fatty acids, antioxidants, and minerals that help reduce inflammation and improve lipid balance, supporting heart health.
- Sunflower seeds are a good source of vitamin E and magnesium, both of which protect vessels from oxidative damage, regulate blood pressure, and support heart function.
- Quince (Cissus quadrangularis):
Helps lower LDL cholesterol, prevent clots, and reduce blood pressure. - Camel thistle:
Cleanses the blood of oxidized cholesterol and improves liver function. - Fennel:
Helps prevent the calcification of fats in the arterial walls.
Nutrients That Support Plaque Stabilization
- Pycnogenol (pine bark extract) and PQQ (pyrroloquinoline quinone):
Help stabilize softer plaque. - Vitamin K2:
Prevents calcium from depositing in the arteries and redirects it to the bones.- The most important sources of this vitamin:
- Natto (Japan): One of the richest foods in K2, especially the MK-7 type made from fermented soybeans. It contains the enzyme nattokinase, useful for reducing blood clotting.
- Grass-fed butter: A good source of K2 type MK-4.
- Differences between types:
- MK-7 (long-acting): Often extracted from natto. Preferred for its extended effect (full day).
- MK-4 (short-acting): Often derived from animal fats. Requires multiple doses per day.
- K2, especially MK-7, is best combined with vitamin D3 to enhance calcium absorption and direct it to the bones rather than the arteries.
- The most important sources of this vitamin:
- Niacin (non-extended-release):
Reduces the thickness of artery walls and improves lipid profile.- Main sources:
- Chicken or beef liver: Among the highest natural foods in niacin content.
- 100 grams of chicken liver contains approximately 13–16 mg of niacin — more than 100% of the daily requirement.
- Grilled chicken breast: An excellent, easy-to-prepare source.
- 100 grams contain about 10–11 mg of niacin, covering most of an adult’s daily requirement.
- These two sources combine nutrient density with high absorption by the body.
- Chicken or beef liver: Among the highest natural foods in niacin content.
- Tocotrienols (a type of vitamin that reduces inflammation and protects artery lining):
- Top dietary sources:
- Red palm oil: One of the richest sources, especially in delta and gamma forms.
- Rice bran oil: Contains both tocotrienols and tocopherols.
- Whole barley rice and acai seed oil: Plant sources rich in antioxidants and overall health support.
- Note: Despite its benefits, tocotrienols are not abundant in the typical diet. Supplements derived from palm oil or rice bran are a viable option for therapeutic doses.
- Top dietary sources:
- Black garlic and berberine:
Improve vascular elasticity and reduce oxidized cholesterol. - Magnesium and potassium:
Relax arteries and improve blood pressure.- Top sources of magnesium:
Almonds, pumpkin seeds (white pulp), raw cacao or dark chocolate (70% and above), leafy greens (such as spinach and kale), avocados, black beans, whole grains (such as oats and quinoa), bananas, and natural yogurt. - Top sources of potassium:
Bananas, sweet potatoes, avocados, spinach, parsley, leafy greens, legumes (such as lentils and beans), dried apricots, beets, natural coconut water, and natural yogurt.
- Top sources of magnesium:
- Vitamin D3:
Reduces inflammation, supports immunity, and slows plaque deposition.- Best source: Sunlight exposure at sunrise or sunset.
- Main sources:
2. Supportive Supplements
- Vitamins B1, B6, B12:
Reduce homocysteine, which is associated with vascular damage. - Vitamin D3 and K2:
A supportive combination for healthy arteries and reduced calcification. - Magnesium supplements:
Help improve vascular relaxation and regulate heart rhythm. - Omega-3 (from fish oil or purslane):
Supports the heart and reduces inflammation. - CoQ10:
Improves energy production in the heart muscle — especially beneficial for those using statin drugs. - Vitamin D (sunlight or supplements):
Activates stem cells and boosts immunity.
Note: It is best to take these supplements under medical supervision, as dosages vary depending on individual conditions. Some may interfere with medications or cause harm if used indiscriminately, especially for those with chronic illnesses or on regular medication.
3. Therapeutic Physical Activity
- Deep breathing exercises to stimulate circulation.
- Cold water immersion to stimulate circulation and activate brown fat and stem cells.
- Daily aerobic exercise (tailored to individual health status).
- Walking after meals to improve blood circulation.
4. Medical Interventions
- Use of cholesterol and blood pressure lowering medications (as prescribed by your doctor).
- Use of blood-thinning medications when needed.
- Medical procedures such as catheterization, stenting, or bypass surgery in advanced cases.
5. Behavioral Modifications
- Sleep regulation using natural herbs such as valerian, and minimizing sleepless nights.
- Manage stress through prayer and deep breathing.
- Avoid smoking, alcohol, and artificial stimulants.
- Practicing prayer with kneeling and prostration stimulates blood circulation and relaxes the nervous system.
Important notes:
- Solenostemma, argel is very useful but should not be overused and is contraindicated with blood-thinning medications.
- Lifestyle is the key to treatment: Nutrition, exercise, sleep and avoiding toxins are more important than drugs alone.
- Stem cell stimulation has become one of the most important prevention and treatment strategies in modern medicine, and it can be activated naturally without drugs through fasting, sports, good sleep, vitamin D, omega-3, and cold water.
👉 Diagnosing Coronary Artery Disease:
Atherosclerosis and coronary artery disease do not appear suddenly, but rather develop silently over years. The key to prevention and early treatment lies in accurate diagnosis, which combines laboratory tests, imaging tests, and functional tests of the heart. In this article, we review the most important tools doctors rely on to assess the health of the heart’s arteries.
Important diagnostic tests include the following:
First: Laboratory tests to assess risk factors
- Blood lipid analysis: Measurement of cholesterol (LDL, HDL) and triglyceride levels, which are key indicators of arterial health.
- High-sensitivity CRP (hs-CRP): Increases in chronic inflammation and is an early hidden indicator of heart disease.
- ApoB: is associated with the number of cholesterol-carrying particles and gives a more accurate assessment of atherosclerosis risk than LDL alone.
- Chromatography of blood sterols: For rare conditions to detect the accumulation of phytosterols, such as sterolemia.
- Genetic tests: Used to identify genetic mutations that increase the risk of lipid disorders or atherosclerosis, especially in familial or early-onset cases.
- Liver biopsy (if needed): May be performed if there are indications that liver disorders affect lipid metabolism.
Second: Advanced imaging and diagnostic tests
- Coronary Calcium Scan (CAC Score): Detects calcium buildup in the walls of the coronary arteries, an important early indicator of atherosclerosis.
- Coronary Angiography: It is considered the gold standard in the diagnosis of coronary artery disease, as it accurately shows the locations and degrees of blockages.
- Magnetic resonance imaging (MRI) or CT scan: It is used to accurately assess the structure of the heart and arteries and detect complications or similar conditions.
Third: Functional tests of cardiac performance
- Electrocardiogram (ECG): Monitors the electrical activity of the heart and detects heart rhythm disorders or ischemia.

- Stress tests: Shows how well the heart performs under physical stress, and helps diagnose angina that may not be apparent at rest.
⚠ When should you call your country’s emergency number?
If you have any of the following symptoms, call an emergency service immediately:
- Chest pain, especially in the center or left side of the chest, that lasts for a few minutes or goes away and then returns. This pain is usually described as pressure, constriction, or a feeling of fullness, and can be mistaken for indigestion or heartburn.
- Discomfort in the upper body, such as: One or both arms, shoulders, neck, jaw, or upper stomach.
- Shortness of breath with or without chest pain
- Nausea or vomiting accompanied by dizziness, lightheadedness or sudden cold sweats.
- These symptoms may be indicators of an impending heart attack and should not be ignored or delay medical evaluation. Quick medical intervention can save your life.
🧠 Interesting facts:
- 80% of heart disease is preventable with a healthy lifestyle.
- Chronic gingivitis is linked to an increased risk of clots!
- Laughter, adequate sleep, and good socialization protect your heart in ways you can’t imagine.
- Natural salt (such as Himalayan salt) is not the enemy… refined sugar is the most dangerous enemy!

Practical recommendations at your fingertips:
- Start with just one step today: Like drinking warm water with lemon in the morning.
- Eliminate one harmful habit: Like too much sugar or too little sleep.
- Adopt the “most and least” rule: Most of your food is natural, and less of your food is processed.
- Be your own first doctor: Keep an eye on your body, and ask for regular checkups.
- Remember: Prevention is not deprivation, it is preservation of your life.
Frequently Asked Questions (FAQ)
- Can you live with coronary artery disease?
Yes, with proper treatment and lifestyle changes, you can live a normal life. - Who is most at risk for coronary artery disease?
- People with diabetes or insulin resistance
- People with high blood pressure
- Those with a family history of heart disease
- Smokers or those who are inactive
- Those with abdominal obesity
- People who eat a lot of processed foods
- What is the difference between angina and a heart attack?
Angina is a temporary pain due to lack of blood flow to the heart, while a heart attack is a complete blockage that can cause damage to the heart muscle. - Do arteries recover?
The arteries will never be the same, but the progression of the disease can be slowed down and partially improved with treatment. - Should I stop working or traveling?
Not necessarily. The doctor decides based on the severity of the condition, and many patients continue their lives normally. - What is the difference between stable and unstable angina?
Stable angina occurs with exertion and is relieved with rest, while unstable angina can occur at rest and is more alarming. - Can I have coronary artery disease without a blockage?
Yes. Sometimes symptoms occur due to causes such as anemia, glandular disorders, or tachycardia, despite the integrity of the arteries. - What is the most serious type of acute coronary syndrome?
ST-segment elevation myocardial infarction (STEMI), because it indicates a complete blockage and requires urgent intervention. - Is Acute Coronary Syndrome always due to a sudden blockage?
Often yes, due to the rupture of a fatty plaque within the artery leading to a blood clot. - How do I differentiate between angina pain and non-cardiac pain?
Angina pain is a pressure or heaviness in the center of the chest, which appears with exertion and goes away with rest.
Non-cardiac pain is sharp or localized and increases with breathing or movement. - Can acute coronary syndrome be prevented?
Yes, by controlling blood pressure, cholesterol, sugar, smoking cessation, and regular exercise.
Conclusion
The heart is the center of life, and the health of our coronary arteries means the health of every cell in our bodies. Coronary artery disease may seem silent at first, but when it’s too late, it’s too loud. Prevention is not a luxury but a necessity, and treatment is not limited to medication, but starts with lifestyle. Understanding the disease is the first step towards overcoming it. Let’s make knowledge and awareness a shield that protects our hearts and the hearts of those we love.

 Turkish
Turkish العربية
العربية








This article was both informative and inspiring—great job!
Fantastic read! 👏 I really appreciate how clearly you explained the topic—your writing not only shows expertise but also makes the subject approachable for a wide audience. It’s rare to come across content that feels both insightful and practical at the same time. At explodingbrands.de we run a growing directory site in Germany that features businesses from many different categories. That’s why I truly value articles like yours, because they highlight how knowledge and visibility can create stronger connections between people, services, and opportunities.Keep up the great work—I’ll definitely be checking back for more of your insights! 🚀